Cell Response to Dental and Orthopedic Materials
To create a healthy environment for the regeneration of periodontal ligament and/or bone around teeth and implants, myriad factors must be addressed. This research details how the surface characteristics chemistry and roughness can affect cell response and local factor production. Providing insight into regeneration at the site of a bony defect, it appears that the surface characteristics of an implant may direct tissue healing and, therefore, result in subsequent implant success by modulating osteoblast phenotypic expression.
Polymers for Drug and Cell Delivery
Most cases of craniosynostosis, the premature fusion of cranial sutures, require surgical reconstruction. In post-operative craniosynostosis patients, bone morphogenetic protein (BMP) inhibitors may be used to prevent rapid bone regrowth, known as re-synostosis. However, this therapy still requires the development of a delivery vehicle to localize release at the administration site. Here, we offer an in situ rapidly crosslinking injectable hydrogel. In addition to craniofacial applications, this hydrogel can potentially provide customizable protein, small molecule, and cell delivery to any site accessible via needle or catheter.
Alginate Microbeads for Stem Cell Delivery
While microencapsulating stem cells in injectable microbeads can enhance delivery and localization, their ability to initiate growth factor production is still unknown. Growth factor mRNA levels and production from alginate microbeads with encapsulated human adipose stem cells (ASC microbeads) cultured in both growth and chondrogenic media were measured over a two-week period. Microencapsulation was found to enhance chondrogenic growth factor production. It was also shown that chrondrogenic medium treatment can decrease angiogenic growth factor production from ASCs, making these cells a potential source for paracrine factors that can stimulate cartilage regeneration.
Matrix Vesicle Microenvironment
1α,25-Dihydroxy vitamin D3 [1,25(OH)2D3] acts on cells through traditional steroid hormone receptor-mediate gene transcription and by initiating rapid membrane-associate signaling pathways. Two receptors have been implicated in rapid signaling by 1,25(OH)2D3, vitamin D receptor (VDR) and disulfide isomerase. To investigate the roles of these two receptors, our lab has established tools including gene knock-out, conditional knock-out, silencing and over-expression in various model systems such as growth plate chondrocytes and extracellular matrix vesicles. Using these models we have demonstrated that Pdia3-dependent signaling in response to 1,25(OH)2D3 regulates growth plate physiology.
The Role of Hormones in Breast Cancer
17β-estradiol can promote the growth and development of several estrogen receptor (ER)-negative breast cancers. ERα36 has been shown to mediate rapid, non-genomic, membrane-associated effects of 17β-estradiol in several cancer cell lines, including triple negative HCC38 breast cancer cells and producing an anti-apoptotic effect. This study provides a working model for a mechanism by which estradiol promotes anti-apoptosis through membrane-associate ERα36, suggesting that ERα36 may be a potential membrane target for drug design against breast cancer, particularly triple negative breast cancer.
The Role of Vitamin D in Osteoarthritis
Post-menopausal women have lower serum 25(OH)D3 metabolism, and sex may be a risk factor in patients with osteoarthritis (OA). Vitamin D is known for its role in bone metabolism, and evidence suggests that vitamin D metabolites mediate inflammation and cartilage remodeling. This study finds that sex differences exist in 25(OH)D3 Vitamin D3 metabolites, which suggests that vitamin D modulation may contribute to the sex differences seen in the severity and development of knee OA.
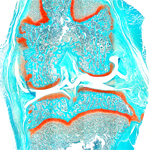
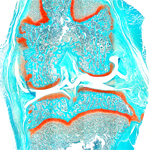
Bone and Cartilage Biology
The secosteroid 1α,25 dihydroxy vitamin D3 acts on cells via classical steroid hormone receptor-mediated gene transcription and by initiating rapid membrane-mediated signaling pathways. Across pathways in the cell’s membrane, these secosteriods interact with protein disulfide isomerase and activate protein kinase C. Recent efforts to determine the signaling proteins in this process have indicated that phospholipase A2 activating protein and Ca2+/calmodulin-dependent kinase II are required.